Health and Lifestyle
Washington state edges closer to a COVID crisis as Thanksgiving arrives
New hospitalizations are spiking as record cases continue to be detected.

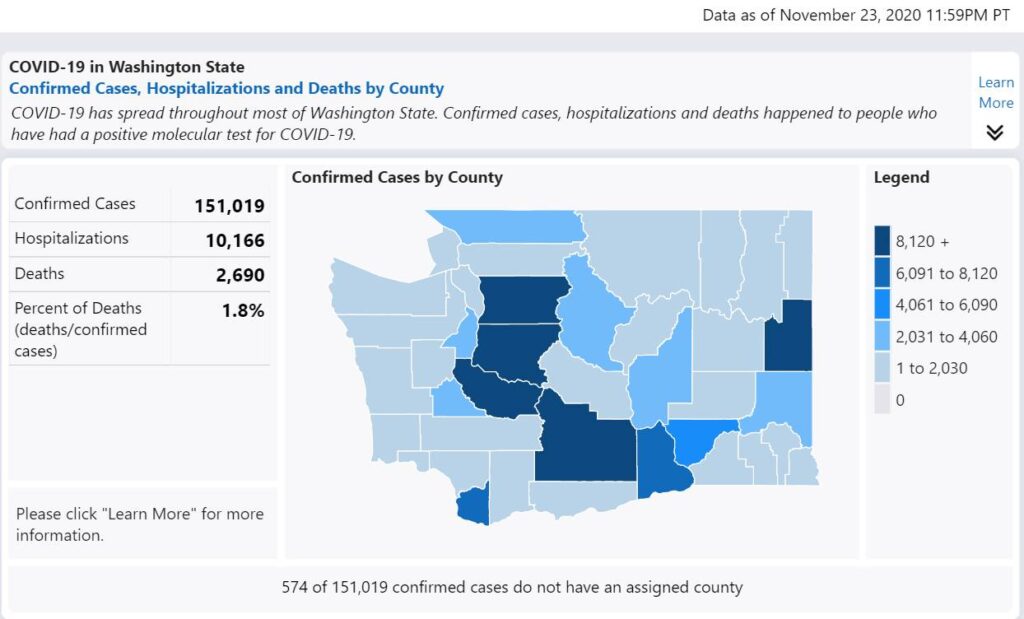
Washington state officials reported that 80 people were admitted to hospitals with COVID-19 yesterday. Detected cases have spiraled to over 2,000 a day, a seven-day moving average. Lines to get tested now stretch for a mile at some locations. Officials have started appealing that only symptomatic individuals get tested. The surge in hospitalization has begun. In a few weeks, the number of fatalities will also begin to increase.
As of this writing, 6.7% of people with a positive test will end up in the hospital, according to the Washington State Department of Health COVID-19 Dashboard. Of those who end up in the hospital, 26.52% will die. We are approaching hospital utilization numbers that are rivaling March-April of 2020 now.
King County is reporting that available resources remain adequate, as does Clark County. In our backyard, Evergreen Hospital has seen the number of hospital patients decline in the last week. Snohomish County is reaching capacity, as are many hospitals in the eastern part of Washington.
The problem isn’t beds; the problem is staff and PPE. The strategic reserve for PPE remains woefully under-supplied despite nine months to prepare. At hospitals, nursing homes, and doctor offices across the country, staff continues to reuse “disposable” PPE items. In Washington, doctors and staff went on strike at MultiCare due to a lack of PPE and officials ignoring even basic safety protocols. Auburn MultiCare, Everett Providence, and Harborview have all had outbreaks within the hospitals and among staff.
Math
The state is adding more than 2,000 cases a day (roughly) 7-day moving average.
Two-thousands cases with 6.7% being hospitalized equal 134 people landing in hospital beds every day in the coming weeks. Hospitalization doesn’t happen instantly but lag one to three weeks behind a detected case. We won’t see the peak of hospitalizations for the cases detected this week for another 7 to 21 days.
Twenty-six-and-a-half percent of hospitalized patients will end up dying from COVID, based on the Washington State Department of Health numbers. That’s 36 people a day when you reach 2,000 detected cases a day. The spike in deaths takes two to six weeks after hospitalization.
A new strain
The primary strain of COVID-19 spreading across the United States is more contagious than the initial strain that arrived here in January. This strain is also apparently less lethal, but it still makes patients extremely sick. Additionally, our understanding of coronavirus has improved. Doctors now approach treatment through the lens of a clotting and inflammation disease, not a pulmonary disease.
While helping improve survivability, it is a double-edged sword. Those who land in the hospital are experiencing prolonged hospitalization, taking up more resources (beds, PPE, staff, medication, equipment) than patients in March.
For the medical community, the smallest mistake around PPE can result in an infection. Those who work with intubated patients face the most dangerous conditions when it comes to exposure.
An anonymous but respected source reported an alarming number of critical care patients on ECMO in Puget Sound. ECMO is the last defense line for the sickest COVID patients, where the lungs have failed, and a machine must replace their function. ECMO is reserved for individuals who were in peak condition before being infected and have some chance of a meaningful recovery.
A worse spike than April
In another two to three weeks, the Washington state hospitals will likely be overwhelmed when you do the math. Complicating things will be Idaho, Montana, and Alaska wanting to fly the sickest of their patients into our region, as they have even fewer resources. By Christmas, the number dying in this state will exceed our worst numbers in March-April. The IHME forecasts that by March 1, 2021, 6,015 Washingtonians will die of COVID, and we’ll experience peak deaths in mid-January.
Business leaders at the major hospital networks are concerned that if capacity is reached, government officials will mandate an end to all elective procedures. COVID taught us that hospitals receive most of their revenue from treating people, not curing people. When treatment programs and elective surgeries were canceled earlier in the year, hospitals faced massive budget shortfalls and were forced into layoffs. All while experiencing a massive increase in costs.
In Washington, hospitals are already deferring some procedures to keep bed utilization lower. So on paper, things look good. The reality is the people being turned away are not people needing hernia repairs, tonsils removed, or cataract surgery. People being turned away right now need heart valve replacements or, in some cases, cancer surgeries.
Unknowns add complexity to treating non-COVID patients
People need to realize that if you are rushed to the emergency room due to a car accident, the staff must assume you are COVID-19 positive when you arrive. Rapid tests are woefully inaccurate. A nasal swab test can take 12 to 24 hours to come back in a hospital setting, under ideal conditions. Until your test results come back, the staff must follow donning and doffing procedures and use up PPE. A doctor wearing a puffer helmet treating an emergency room patient can’t go and examine another patient until they remove the equipment. For anesthesia, a doctor might move between three different rooms under normal circumstances. With COVID, they are anchored to one room if they don’t know the patient’s COVID status. Now another doctor has to be called in to support any other patients. This is the same for nurses, technicians, and specialists.
The coming crisis
When you add it up:
- 2,000 cases a day results in
- 134 new hospitalizations in one to three weeks
- 36 deaths from that group in three to six weeks
- Hospitalization lasts 10 days conservatively
- Equals 1,340 COVID patients in the hospital, conservatively
- 26% of those patients critically ill
That’s conservative math based on the existing information we have. It’s too late (which isn’t to say we should do nothing) to stop this COVID train.
The grim reality is you don’t want to get sick around the third week of December. To get ill with COVID around that time indicates your exposure was around Thanksgiving. You may find yourself or a loved one in a rationed care situation. When care is rationed, patients are given a score based on their age, comorbidities, condition, and how much lifespan they have left. If you don’t get a good enough score, your treatment may be a morphine drip to provide a comfortable end of life. When care is rationed, you or a loved one could end up in the hospital for something non-COVID related, such as an accident, stroke, or heart attack. The same formula will be applied, not because of a lack of beds, but a lack of staff.
They are doing rationed care in Utah, parts of Texas, and North Dakota. In North Dakota, COVID positive medical personnel who are asymptomatic can continue to work because of staffing shortages. When staff who have coronavirus continue to work, they endanger the non-infected team working with them, creating a cycle of shrinking resources. Idaho is on the brink of rationing care, with no political will to slow the surge in their state. Part of the plan in Idaho is to send their patients to Seattle and Portland, Oregon, straining resources further.
There is no way to prevent the coming tidal wave of patients for Washington state, but we can avoid going to rationed care as we inch closer to the end of the year. Everyone needs to choose very wisely in the next 24 hours.










